Achilles Tendonitis
Background
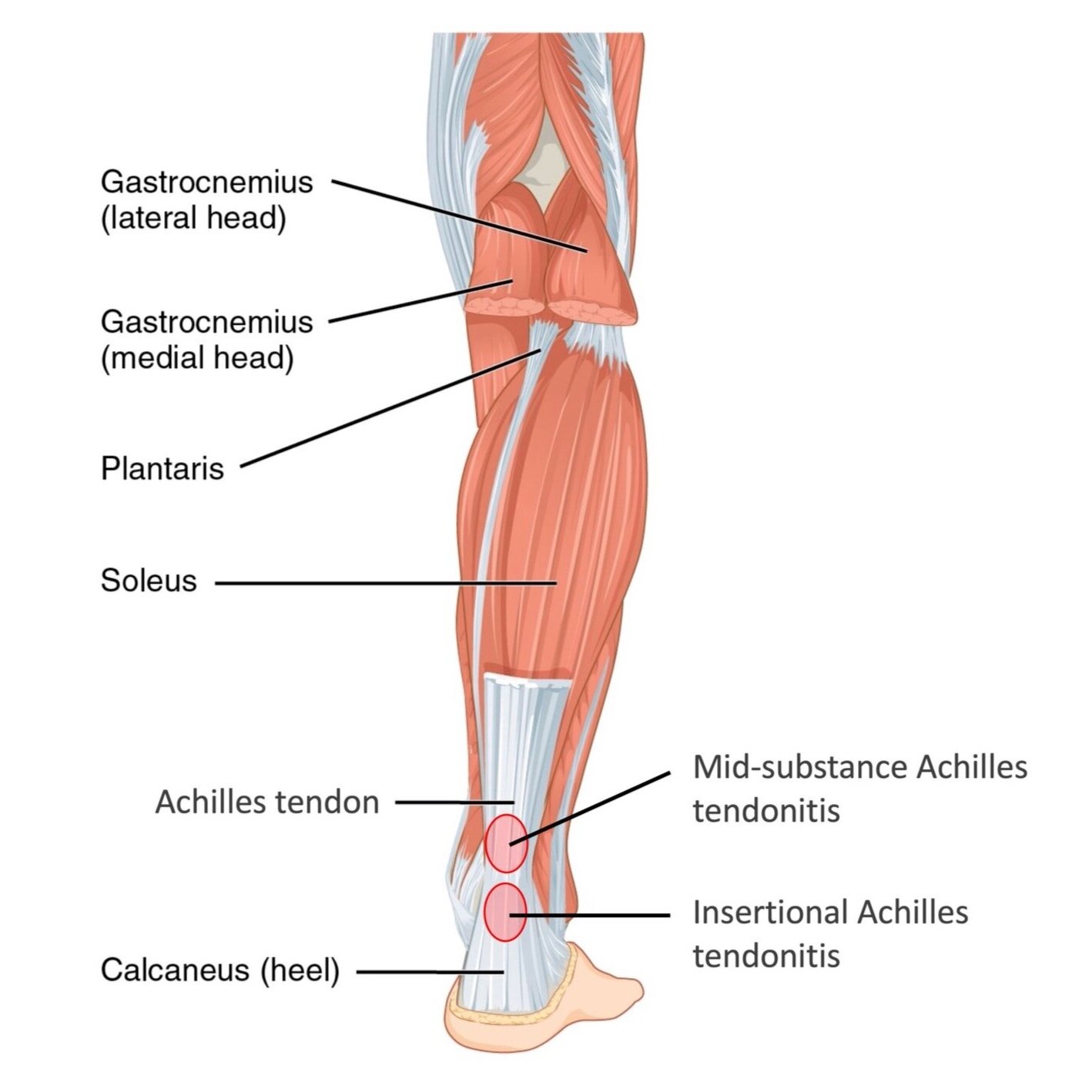
The Achilles tendon is the largest and strongest tendon in your body. It attaches the calf muscles (gastrocnemius and soleus) to your heel bone (calcaneus) and is important during the push-off phase of gait. It is also critical for jumping and stair climbing, and for activities like running or playing tennis.
Achilles tendonitis is inflammation of that tendon. At first, fluid simply collects around the outside of the tendon, causing discomfort. This early stage is usually reversible with rest, ice, stretching, and non-steroidal anti-inflammatory medication. However, if the tendonitis persists, chronic changes begin to occur within the tendon. These include tendon thickening, loss of the normal longitudinal structure of the tendon’s fibrils, tendon weakening, and micro-tearing of the tendon.
There are two distinct forms of Achilles tendonitis. The first form is called “insertional tendonitis.” This occurs at the most distal part of the tendon, right as the tendon attaches to bone. Patients with insertional tendonitis usually have an enlarged posterior-superior corner of the calcaneus called a “Haglund’s deformity.” This bony prominence puts increased pressure on the tendon as it passes by. Additional calcification often forms within the attachment of the unhealthy tendon, causing a “bone spur.” Patients can often feel the Haglund’s deformity and bone spur on their heel, where they create difficulty with shoe wear. As a result, the prominence has become colloquially known as a “pump bump.”
The second form of Achilles tendonitis is called “mid-substance tendonitis.” This occurs an inch or two higher up on the tendon and is not associated with a bony deformity. In these cases, the tendon becomes particularly swollen and thickened due to an area of diminished blood supply. Tendon degeneration results in micro-tearing and tendon elongation, weakening, and pain. The bump is usually above the heel of the shoes, so patient symptoms come not from contact with shoes but simply from stretching of the tendon during the push-off phase of gait.
Imaging
At your first visit to the clinic, Dr. Bohl will obtain x-rays of your foot and ankle. If you have the insertional type of Achilles tendonitis, this will confirm the Haglund’s deformity and often show bone spurs within the tendon. In general, Dr. Bohl will recommend an initial attempt at conservative management prior to obtaining an MRI. However, if the symptoms persist, Dr. Bohl will recommend an MRI of the ankle. On MRI, the Achilles tendon is inflamed and thickened, with surrounding fluid. This presents as a radiographic expansion and graying seen within the tendon on sagittal cuts of the MRI.
Nonsurgical treatment
Dr. Bohl encourages patients to work hard at nonsurgical treatment for Achilles tendonitis. The majority of patients can cure the condition with a guided and focused nonsurgical treatment plan. Depending on the duration, severity, and type of your symptoms, your physical exam, and your personal goals and responsibilities, Dr. Bohl will tailor his treatment plan to you. The general structure of treatment includes:
Phase 1: Reduce the inflammation (2 weeks)
Immobilization (boot)
Anti-inflammatory medication (meloxicam, Voltaren gel)
Activity modification (rest)
Ice at the end of the day
Phase 2: Rehabilitation (6-12 weeks)
Formal physical therapy and/or home exercise program
Calf stretching program
Eccentric Achilles strengthening
Continue the anti-inflammatory medication (meloxicam, Voltaren gel)
Phase 3: Injection (only if not resolved by phase 2)
Platelet-rich plasma (PRP) injection into tendon
Platelet rich plasma
Platelet rich plasma uses your body’s own progenitor cells to decrease inflammation and regenerate tissue.
Platelet rich plasma (PRP) injection deserves special mention as a nonsurgical option that is increasingly popular with patients. This treatment provides your own body’s progenitor cells with regenerative potential directly into the diseased tissue. Laboratory evidence shows that PRP injection decreases inflammation and leads to tissue healing in multiple areas throughout the musculoskeletal system.
This procedure is performed in the office at a routine patient visit. A small amount of blood is drawn, just like for a routine laboratory blood draw. This is spun down in a centrifuge and filtered for the cells with the most regenerative potential. These cells are provided carefully and accurately to the affected tissue using ultrasound guidance. The injection itself takes about one minute and is no more painful than any routine musculoskeletal injection.
Patients are encouraged to take it easy for the first few days following this procedure, but have no specific limitations. They can walk out of the clinic in regular shoes. Patients may feel some relief immediately, but most of the benefits accrue during the subsequent weeks and months.
Surgical treatment
Surgical treatment for insertional Achilles tendonitis
There is no rush to do surgery for Achilles tendonitis. Patients can continue nonsurgical treatment and symptom management for as long as they want. However, if and when patients do decide they are ready, there are excellent surgical options for Achilles tendonitis that provide marked relief. The surgical treatments differ between insertional tendonitis and mid-substance tendonitis, as follows:
For patients with insertional tendonitis, the main problem is the Haglund’s deformity irritating the tendon. A small incision is made on the back of the ankle. The unhealthy, inflammed, and painful portion of the Achilles tendon is removed as part of the surgical approach to the Haglund’s deformity. Bone spurs are removed as well. The Haglund’s deformity itself is then removed, leaving new healthy bone with smooth edges that won’t irritate the tendon. The Achilles tendon is then re-secured to the calcaneus in a slightly shortened manner as to remove tension and enhance the strength of the repair.
Surgical treatment for mid-substance Achilles tendonitis
For patients with mid-substance tendonitis, so much of the Achilles tendon is usually unhealthy that we recommend borrowing another tendon from the foot — the flexor hallicus longus — to add strength to the reconstruction. A small incision is made on the back of the ankle and the flexor hallicus longus is retrieved. The unhealthy, inflammed, and painful portion of the Achilles tendon is removed, and the flexor hallicus longus is transferred from its pathway to the big toe into the calcaneal tuberosity. The Achilles tendon is then repaired and strengthened using the intervening flexor hallicus longus tendon to add strength for running, jumping, and the push-off phase of gait.
In both types of reconstruction, the postoperative plan is similar. Patients are in a splint for 2 weeks (using knee scooter or crutches), a cast for 4 weeks (using knee scooter or crutches), and finally a boot for 4 more weeks (walking allowed). Physical therapy is initiated at the 6th postoperative week.
Patients do very well following Achilles tendon reconstruction for chronic tendonitis. Dr. Bohl will be very happy to discuss the risks and benefits of surgery and how the rehabilitation can be worked into the demands of your life.